S.R. & A.C. equally contributed
Background: Despite significative improvements in the management of FLT3-mutated AML and its prognosis since FLT3 inhibitors ( FLT3i) adoption, a significant proportion of patients results refractory or ultimately relapses after this targeted treatment. Gilteritinib is an oral and selective FLT3i with single-agent activity as salvage therapy in Relapsed/Refractory patients (R/R). The investigation of resistance mechanism to Gilteritinib is crucial to guide next therapeutic choices and improve drug effectiveness. Thus far, correlative studies have elucidated mainly intrinsic and mutational resistance mechanisms. However, less is known regarding potential extrinsic mechanisms and about the role of the immune system in influencing this FLT3i activity. Herein, we aimed at investigating intrinsic as well as novel extrinsic (immunological) mechanisms of resistance to Gilteritinib in routine clinical practice.
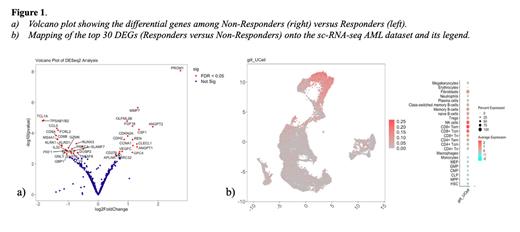
Methods: A cohort of FLT3-mut AML patients treated with Gilteritinib at Hematology Institute of Bologna was selected. DNA/RNA were extracted from bone marrow (BM) samples pre-therapy and at first response assessment and screened by a custom NGS panel covering the full-coding sequence of 28 genes and a NanoString gene-expression analysis using the PanCancer IO 360 Panel. Data were collected in accordance with GCP and Helsinki declaration. NanoString data were acquired and analyzed using the nCounter FLEX Analysis System and the nSolver advanced analysis module (version 2.0.115). DESeq2 multi-factor design was employed to account for potential confounders. A public sc-RNA-seq dataset of newly diagnosed AMLs (Dufva et al. Cancer Cell 2020) was used to map DEGs between Responders and Non-Responders to Gilteritinib onto reference AML BM samples. Single-cell gene expression scores were computed using the UCell package in R.
Results: Overall, 20 FLT3-mutated R/R AML patients receiving Gilteritinib as single-agent therapy were enrolled in this study. The median age at Gilteritinib therapy was 62 (range 33 - 77) years and 13/20 (65%) patients were male. Seventeen out of 20 (85 %) patients harbored a FLT3-ITD mutation, 2/20 (10 %) a TKD mutation and 1 (5 %) patient both mutations. Eleven out of 20 (55 %) patients had a concomitant NPM1 mutation. Patients were dichotomized into Responders (R) (n=9) and Non-Responders (NR) (n = 11) according to BM response.
Intrinsic mechanisms of resistance were evaluated by NGS analyses on 13 patients (R=7 and NR=6). Firstly, FLT3 full-coding sequencing did not detect any clearly pathogenetic Non-Canonical (NC) mutation: M737I, M837I, P890L and P534L were four detected NC variants with a possible role in FLT3i sensitivity, however their low VAF (1-2 %) suggests a “passenger” role in this cohort. Secondly, evaluating variations in VAF of non- FLT3 variants detected pre- and post-therapy we observed a new variant onset in 4/6 (66.7 %) Gilteritinib NR patients, affecting genes involved in RAS pathway in all cases (1 NRAS, 2 KRAS and 1 PTPN11).
Significant differences in immune transcriptional profiles were observed when comparing R and NR patients (R = 9 and NR = 11), including higher expression of genes reflecting T/NK function ( CD8A, GZMK, KLRK1, GNLY) and, more specifically, T-cell activity ( PRF1, EOMES, ZAP70, TNFSF8) in responders. Conversely, oncogenes involved in MAPK/Akt ( PROM1, ANGPT1, ANGPT2) or cell-cycle regulators ( CDKN2A, CCNA1) were overexpressed in NR patients (Fig. 1a). We next selected the top 30 DEGs between R and NR and we averaged gene expression across all BM samples. Gene set enrichment analysis (GSEA) revealed that approximately 25% of the significantly enriched pathways when using the top 30 DEGs as input were related to T-cell function / TCR signaling. By projecting the top 30 DEGs genes onto a sc-RNA-seq map of the AML tumor microenvironment, we found that they were largely expressed by CD8 + T EM, CD8 + T CM and NK cells (Fig. 1b).
Summary/Conclusion: This study confirmed evolutionary trajectories often involving RAS pathway mutations as an intrinsic mechanism of resistance to Gilteritinib therapy. Of note, differences in immune transcriptomic profiles, involving mainly CD8+ T-Cells and NK-Cells, were associated with response, pointing to a previously unappreciated role of the immune system in mediating response to Gilteritinib.
Disclosures
Papayannidis:Abbvie, Astellas, Servier, Menarini/Stemline, BMS, Pfizer, Amgen, Janssen, Incyte, Novartis: Honoraria; Pfizer, Astellas, Janssen, GSK, Blueprint, Jazz Pharmaceuticals, Abbvie, Novartis, Delbert Laboratoires: Membership on an entity's Board of Directors or advisory committees. Cavo:Takeda: Honoraria; GlaxoSmithKline: Honoraria; Adaptive: Honoraria; Sanofi: Consultancy, Honoraria; Roche: Honoraria; Amgen: Honoraria; AbbVie: Consultancy, Honoraria; Celgene/Bristol Myers Squibb: Consultancy, Honoraria, Speakers Bureau; Janssen: Consultancy, Honoraria, Speakers Bureau. Curti:Pfizer: Membership on an entity's Board of Directors or advisory committees; Novartis: Membership on an entity's Board of Directors or advisory committees; Abbvie: Membership on an entity's Board of Directors or advisory committees.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal